- 0
- 1
- 2
- 0
- 1
- 2
- 3
- 4
- ,
- 0
- 1
- 2
- 3
- 4
- 5
- 0
- 0
- ,
- 0
- 0
- 0
The HIV epidemic in Australia is largely in men who have sex with men, with over 2/3 of new transmissions occurring in this population (this rate has remained stable in the past 10 years). Harm reduction strategies among injection drug users have been successful in lowering transmission among this group. The rate of maternal transmission in Australia is extremely low as a result of medical interventions. HIV among women involved in sex work is among the lowest in the world in Australia with no new cases reported in 2015.
The rate of HIV cases among Aboriginal and Torres Strait Island peoples, particularly males, has been on the rise in the past 5 years.
This data highlights some of the successes in lowering HIV transmission in Australia, however given that ¼ of HIV transmissions among heterosexuals occur in people who are from countries where HIV Is endemic, more targeted targeted programming, education and health policy changes must be undertaken to provide care and resources for this population..
-MIGRANT POPULATIONS
MIGRANT POPULATIONS
AND HIV
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- .
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- M
- i
- l
- l
- i
- o
- n
- 0
- 1
- 2
- ,
- 0
- 1
- 0
- 1
- 2
- 0
- 1
- 2
- 3
- 4
- 5
- 6
- U
- n
- k
- n
- o
- w
- n
- U
- n
- k
- n
- o
- w
- n
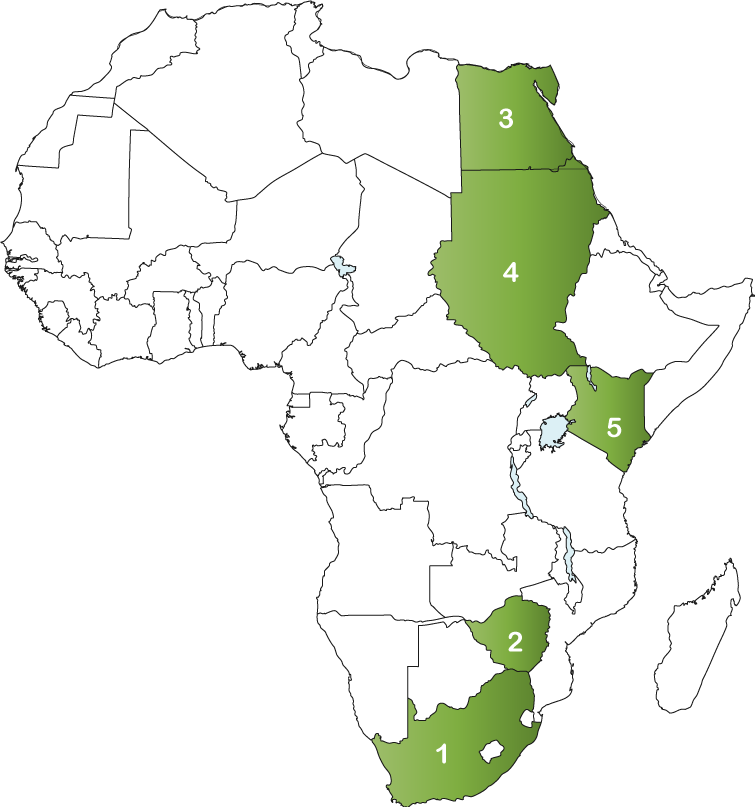
TOP 5 AFRICAN COUNTRIES
OF ORIGIN FOR MIGRANTS IN AUSTRALIA
- 1. South Africa: 183,370
- 2. Zimbabwe: 38,843
- 3. Egypt: 45,352
- 4. Sudan: 23,989
- 5. Kenya: 17,850
-TOTAL POPULATION
PEOPLE LIVING WITH HIV
- 0
- 1
- 2
- 0
- 1
- 2
- 3
- 4
- 5
- ,
- 0
- 1
- 2
- 3
- 0
- 1
- 0
- 1
- 2
- 3
NEW INFECTIONS
- 0
- 1
- ,
- 0
- 0
- 1
- 2
- 0
- 1
- 2
- 3
- 4
- 5
HIV TREATMENT CASCADE
KEY AND AFFECTED POPULATIONS
16% of new diagnoses
68% of new infections
3% of new diagnoses
There are about 20,000 sex workers in Australia. In 2016, The Australian Institute of Criminology and the Scarlet Alliance (Australian Sex Workers Association) surveyed 594 sex workers across Australia, 412 of whom were migrants. Most were female, with only 17 male and eight transgender respondents. Of the identified migrant survey population, 44 percent indicated they were born in Thailand, 26 percent in China, nine percent in South Korea and five percent in New Zealand. Thai, Chinese and Korean-speaking migrants were specifically targeted for survey collection). 16% of those surveyed were born in a country other than Thailand, China, Korea and New Zealand. This includes people born in South Africa and Zimbabwe.
While the majority of HIV diagnoses in Australia are among Australian residents, and primarily amongst gay men, in some jurisdictions such as Western Australia, HIV among internationally mobile communities comprises more than 50% of new diagnoses.
HEALTH
There is a perception that Australia tests people for HIV with the aim of banning the entry of HIV-positive people as a result of the country’s travel and/or migration restrictions. While the policy rationale for restricting entry to people with HIV is said to be an economic one, the perception that Australia bans entry to people living with HIV perpetuates the sentiment that they are not welcome and may increase HIV-related stigma among new migrants.
Migrants may be exposed to health risks before, during and after they leave their countries of origin. The migration journey for HIV-positive migrants in Australia is fraught with barriers that include discrimination, marginalization and lack of knowledge about how to access health services.
There are a range of policy interventions that could be developed to address barriers and the lack of coordination across health care services for migrants, refugees and asylum seekers in Australia.
Barriers to health care access include:
- Long wait times for services, especially Emergency Departments visits in public hospitals,
- Cost of services, especially for specialist and dental health care,
- Navigating the health system,
- Lack of interpreters and female physicians, and specialist care
- Instances of discrimination,
- Other needs, such as income generation, taking precedence, particularly in cases where refugees or migrants are employed in casual or temporary work with no leave provisions.
Australia’s National Strategic Plan 2014-2017 reported that barriers to HIV service included:
- Lack of resources,
- Stigma and discrimination, and
- Inadequate amount of culturally appropriate services and initiatives.
There is a need for HIV messaging and customized testing and treatment options to better meet the needs of persons originating from countries with high HIV prevalence.
POLICY
Australian health care policy for refugees and asylum seekers is complex and directly tied to immigration policy. Health care policy for refugees who enter the country through the Humanitarian Program is comprehensive; providing refugees access to Medicare, early health assessment, specialized torture and trauma services, and access to the same services as other Australians. Migrants, refugees or asylum seekers who enter Australia through “unauthorized” channels or who enter on a range of visa types are subject to fragmented health care policy. 40% of asylum seekers in Australia have no access to medical care.
In general, policy making on migration and health is developed within silos that often have different goals. For example, increasing foreign labour requirements while imposing restrictions on migrants can negatively impact the health of migrants. Policy coordination across the health, labour and immigration sectors may create policies that address the health and social welfare of migrants in their destination countries.
Australia’s policy response to HIV and migration has been reactive with no coordinated policy or program response. This is largely the result of the poorly understood relationship between HIV and migration, stigma, racism, marginalization, evolving migration policies and labour mobility.
Given that Australia is one of several high income countries experiencing a disproportionate number of new HIV diagnoses among people from high prevalence regions, particularly from sub Saharan Africa and South East Asia, an integrated response across government, community, health services and research is necessary to address this issue.
THE RESPONSE
In light of HIV transmission patterns in Australia, priority action in tackling transmission among persons born in sub-Saharan Africa should be taken in the areas of targeted health promotion and education initiatives. These initiatives should be designed to create better awareness among individuals born in sub-Saharan Africa and their partners about the need for consistent testing and early treatment seeking for infected persons. However, since access to health care services and treatment is not extended to every person residing in Australia, more information and navigation supports should be put in place to help HIV-infected individuals access Australia’s health care services.
Founded in 2002, the Global Fund is a partnership between governments, civil society, the private sector and people affected by AIDS, malaria and tuberculosis. The Global Fund raises and invests nearly US$4 billion a year to support programs run by local experts in countries and communities most in need.
Each implementing country establishes a national committee, or Country Coordinating Mechanism, to submit requests for funding on behalf of the entire country, and to oversee implementation once the request has become a signed grant. Country Coordinating Mechanisms include representatives of every sector involved in the response to the diseases.
South African migrants represent the highest migrant group in Australia. Please click here for South Africa’s Country Coordinating Mechanism.
-SOURCES
- https://www.afao.org.au/library/hiv-australia/volume-12/vol.-12-number-2/australia-migration-and-hiv-an-evolving-policy-landscape#.WHultbYrK9Z
- https://www.afao.org.au/about-hiv/hiv-and-the-law#mig.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1282570/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1282570/
- https://www.afao.org.au/library/hiv-australia/volume-13/HIV-Australia-13-1-2020-targets/hiv-and-mobility-in-australia-roadmap-for-action#.WHum0bYrK9a
- http://www.unaids.org/sites/default/files/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_US_Narrative_Report.pdf
- http://countrymeters.info/en/Australia
- http://www.iom.int/world-migration
- https://kirby.unsw.edu.au/sites/default/files/hiv/resources/2015%20Annual%20Surveillance%20Report%20of%20HIV,%20viral%20hepatitis,%20STIs.pdf
- http://www.hivmediaguide.org.au/hiv-in-australia/hiv-statistics-australia/
- https://data.kirby.unsw.edu.au/
- https://data.kirby.unsw.edu.au/hiv
- http://www.aic.gov.au/publications/current%20series/rpp/121-140/rpp131/07_migrant_sex_workers.html
- http://scanlonfoundation.org.au/wp-content/uploads/2016/11/2016-Mapping-Social-Cohesion-Report-FINAL-with-covers.pdf
- http://www.unaids.org/en/resources/documents/2017/20170720_Data_book_2017